Appreciation of mass spectrometry application case | Identification of Legionella in “high-risk latent patients”
Nov 17,2023 Zybio News
01/ Case description
A senior patient was admitted to our hospital because of oppression and discomfort in chest and sudden stethalgia. The patient was diagnosed as aortic dissection, kidney transplantation and grade 3 hypertension (extremely high risk). According to the diagnosis at admission, the patient was treated with aortic valve related surgery and open-heart surgery assisted by cardiopulmonary bypass in time, and was monitored in ICU after the surgery. On the morning of September 7, the patient's blood pressure dropped, accompanied by high fever, shortness of breath, cyanosis at the end of limbs and low skin temperature. The laboratory examination of the patient showed that PCT increased sharply (from 3.61 to 44.39), which was considered cardiogenic shock complicated with infection.
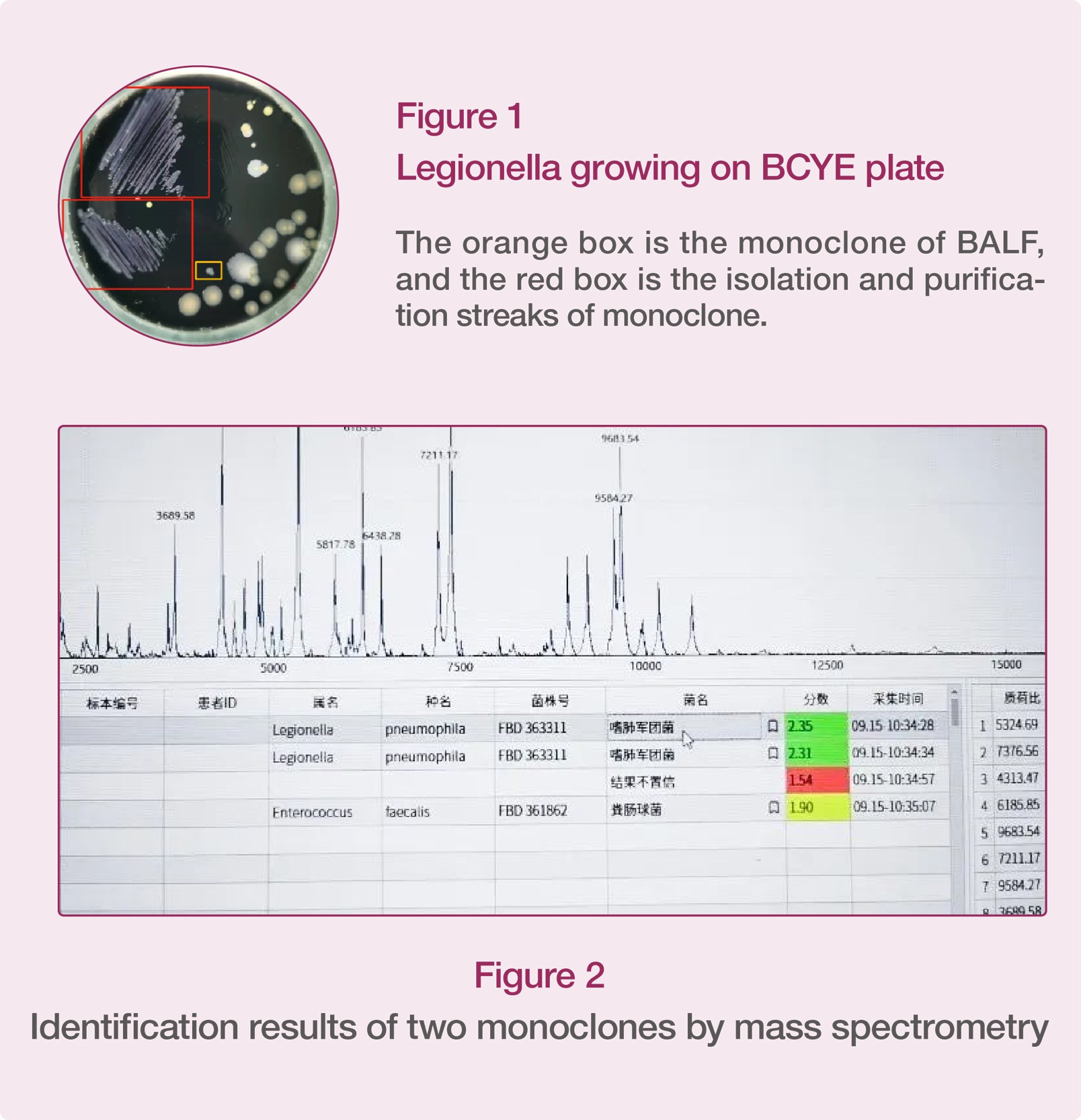
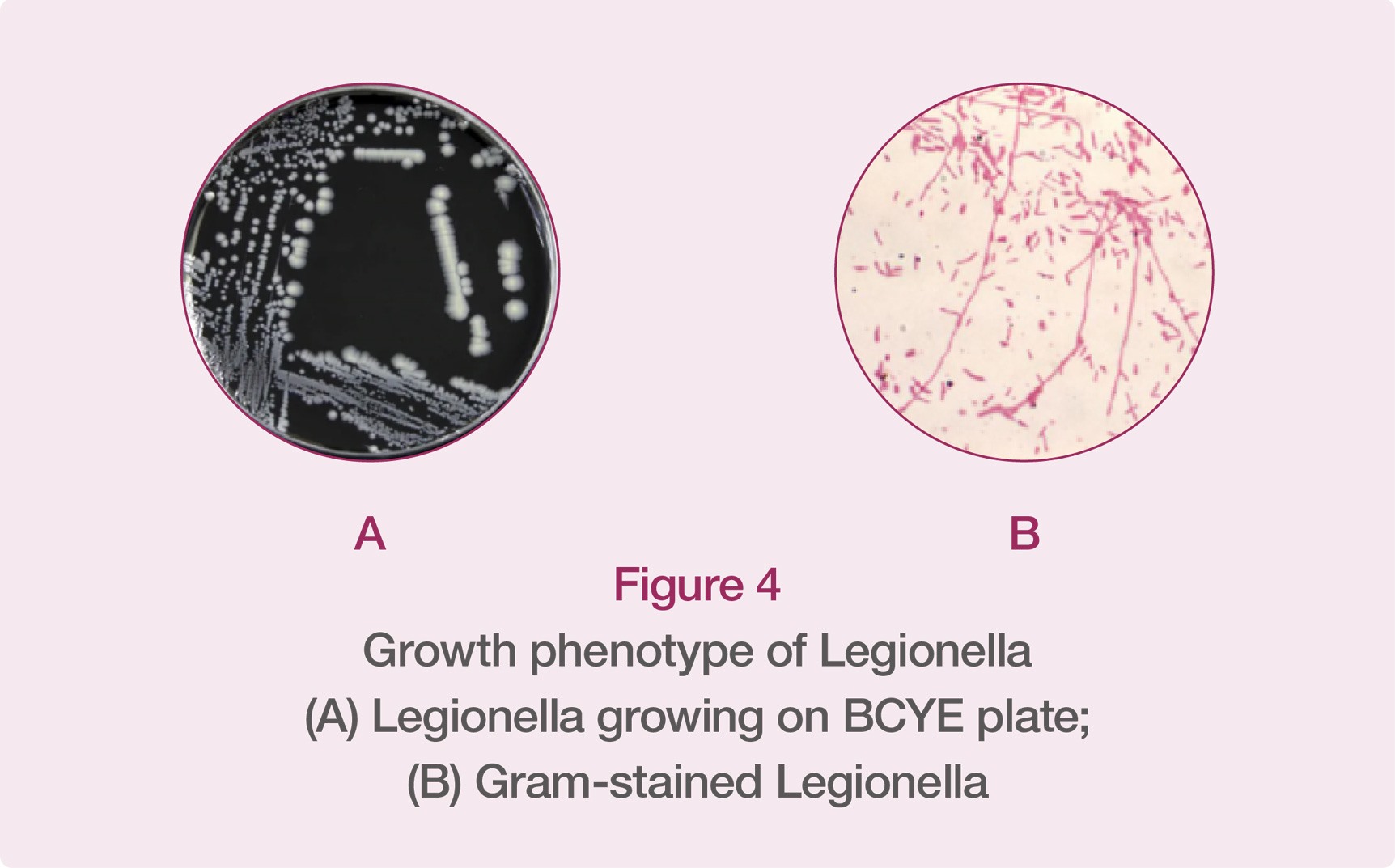
The patient was given broad-spectrum anti-infection treatment. By drawing blood for sample culture and collecting bronchoalveolar lavage fluid (BALF) for pathogen testing, no gram-positive cocci or fungi were found in the culture results. The patient was initially diagnosed as Legionella pneumophila infection through the detection of IgM of respiratory pathogen. The BALF was isolated for culture in BCYE agar, and two tiny gray-white protruding colonies were successfully isolated and cultured (Figure 1). Then, the monoclone of the suspected pathogenic bacteria was identified by Zybio’s EXS series mass spectrometer, confirming that the patient was infected by Legionella pneumophila (Figure 2).
The patient was rather old and was complicated with multiple underlying diseases, his disease had an acute and severe onset and progressed rapidly. If the pathogenic microbe was identified with a conventional identification method, it may delay the effective treatment of the patient. As a result, the EXS series mass spectrometer was used to identify the pathogenic microbe, it quickly and accurately diagnosed the source of infection, helping the patient get timely and effective treatment.
02/ Discussion
In the conventional microbiology laboratory, the cultures isolated from patients' specimens by culture techniques are mainly identified by biochemical and serological tests (such as TPPA). Legionella, as fastidious bacteria, has multiple species. Therefore, it is impossible to identify Legionella through conventional biochemical reactions. Some common pathogenic Legionella can be identified to the species level through tests such as colony autofluorescence, culture medium browning test, Hippurate hydrolysis, gelatin liquefaction, enzyme contact and oxidase [5]. TPPA test is usually used to classify Legionella isolates, but negative or unclear results are frequently seen [6]. In most cases, the quality of the testing results depends on the experience of the laboratory staff.
As the standard method is a laboratory-intensive, time-consuming, and easy to generate false negative results, many molecular techniques have been developed to detect Legionella [7, 8]. Although the molecular approach is sensitive and specific, it is rather expensive and requires a specialized laboratory and well-trained staff. In addition, as the conventional DNA detection method cannot distinguish between dead bacteria and live bacteria during the identification of environmental microbes, there is no correlation between the test results and the actual bacterial load, so it is impossible to quantify the actual risk brought by the bacteria to human beings. Therefore, the testing method based on culture is considered as a reference method for environmental monitoring of Legionella [9]. Therefore, it is necessary to develop a rapid and low-cost method to support the culture technique, to improve the diagnostic efficiency and assist the clinicians to adopt appropriate antibiotics for treatment.
However, with the introduction of mass spectrometers to clinical labs, microbes can be identified more quickly. Mass spectrometer is easy and convenient to operate, with higher detection rate, shorter detection time and lower detection cost. In addition, mass spectrometer can also support traceability analysis of microbes and solve the difficult problem of rapid and accurate identification of microbes at present. Therefore, it has been widely used in microbial identification in clinical practices.
03/ Clinica significance
Legionella, also known as "Legionnaires' disease", first broke out in 1976 during a convention of the American Legion, Philadelphia USA, with 221 people infected and 34 people dead. The pathogen was isolated from autopsy tissue and named Legionella [1].
Legionellosis is a very serious and even fatal pneumonia. According to the estimation of WHO, the incidence of Legionellosis is close to 100,000 cases per year in western countries, and the main infection route is the inhalation of contaminated aerosol (Figure 3).

Legionella is generally susceptible to people of all ages, especially to the elderly. In this regard, according to the survey of community-acquired pneumonia among urban adults in China showed that, the incidence of Legionella pneumonia was 5.9% among people aged over 65 years, and only 2.9% among those aged under 65 years. Host risk factors leading to Legionella pneumonia include male, smoking, chronic cardiopulmonary disease, diabetes, end-stage renal failure, complicated with tumor and immunosuppression, etc. [2]
04 / Diagnostic criteria of Legionella
Legionella is an important cause of community acquired pneumonia (CAP). According to the literature, there were cases of treatment failure of Legionella infection, among which delayed medical treatment or untimely and inappropriate antibacterial treatment may be the main reasons for the failure of treatment of Legionella pneumonia. Therefore, it is crucial to identify Legionella infection in the early stage, because it directly affects the timing and therapeutic scheme of empirical antibiotic treatment and effectively reduces the risk of adverse consequences.
Currently, there are 52 species, 3 subgroups and 70 serotypes of Legionella, and 24 species of Legionella are related to human diseases. The most common one is Legionella pneumophila, which mainly leads to Legionella pneumonia [3]. According to the Guidelines for the Diagnosis and Treatment of Adult Community Acquired Pneumonia in China (2016 Edition), the testing results that can be used as the basis for etiological diagnosis are as follows:
(1)Legionella isolated and cultured from qualified lower respiratory tract specimens, pleural effusion, bronchial mucosa biopsy specimens or lung biopsy specimens;
(2)Positive result of Legionella pneumophila type I urine antigen test (ICT method);
(3)A 4-fold or more rise in the titer of paired sera Legionella pneumophila type I specific antibody (IFA method or ELISA method) in acute and recovery stages
Among them, the positive result of Legionella culture is the gold standard for the diagnosis of Legionella infection, but the positive rate is low, and the early use of antibiotics may lead to false negative result. Using BALF and lung biopsy samples can improve the positive rate [4].
Legionella is a kind of gram-negative aerobic bacterium that needs special nutrients. As it requires harsh culture conditions, it only grows slowly on a special medium called F-G agar containing iron phosphate and L-cysteine or buffered charcoal yeast extract (BCYE) in air containing 2.5% CO2 at pH 6.0 ~ 6.9 and 35℃, with small colonies showing brown pigmentation (Figure 4).
References
[1] Legionella (Legionnaires' Disease and Pontiac Fever).CDC. January 15, 2016 [21 March 2016].
[2] GreenbergD, Chiou C C, Famigilleti R, et al. Problem pathogens: paediatriclegionellosis—implications for improved diagnosis[J]. The Lancet infectiousdiseases, 2006, 6(8): 529-535.
[3] 梁思聪,陈愉.军团菌肺炎的诊治策略[J].中国实用内科杂志,2020,40(5):357-361.
[4] 中华医学会呼吸病学分会. 中国成人社区获得性肺炎诊断和治疗指南(2016年版) [J] . 中华结核和呼吸杂志,2016,39 (4): 253-279. DOI: 10.3760/cma.j.issn.1001-0939.2016.04.005
[5] 朱庆义. 临床与环境标本中的军团菌检验方法学 [J/CD] . 中华临床实验室管理电子杂志,2016,4 (1): 18-25.DOI: 10.3877/cma.j.issn.2095-5820.2016.01.005
[6] Orsini M, Cristino S, Grottola A, et al. Bacteria misagglutination inlegionella surveillance programmes[J]. 2011, 179-180.
[7] Templeton K E, Scheltinga S A, Sillekens P, et al. Development and clinicalevaluation of an internally controlled, single-tube multiplex real-time PCRassay for detection of Legionella pneumophila and other Legionella species[J].Journal of Clinical Microbiology, 2003, 41(9): 4016-4021.
[8] Blyth C C, Adams D N, Chen S C A. Diagnostic and typing methods forinvestigating Legionella infection[J]. New South Wales public health bulletin,2009, 20(10): 157-161.
[9] Lee J V, Lai S, Exner M, et al. An international trial of quantitative PCR formonitoring Legionella in artificial water systems[J]. Journal of appliedmicrobiology, 2011, 110(4): 1032-1044.

